| |
 |

For IBS Diarrhea, Constipation, Pain, & Bloating!
Stock Up! Save On All
Tummy Care Favorites!
Have you seen our
new IBS Quick Tips?
|
 |
|
| |
September 4, 2013 ~ Scroll down for full newsletter or follow the links:
Share!
 
Ask Heather »
Hormones and IBS? Menstruation, Pregnancy, Menopause, & More.
Special Letter »
Andrea Says, Don't Go Anywhere Without Them!
IBS Recipe »
Maple Glazed Tuna - Tastes Fancy, Made Simple!
News & Research »
Soy Foods Protect Against Colon Cancer
»
Is Going Gluten-Free Right for You?
»
Science Finds How Peppermint Relieves IBS (it's interesting!)

|
|
Have questions? Call toll free (866) 640-4942.
Outside the US (206) 264 8069.
Enjoy the newsletter!
Heather Van Vorous & Heather's Tummy Care
Over 10 Years of IBS Business!
|
Did a friend send you this newsletter? Sign up here for your own free subscription.

Fancy-Simple Maple Glazed Tuna This is a great recipe that only tastes rich and sophisticated. It's actually super fast and easy to make with basic pantry staples. You can substitute salmon, or a meatier white fish such as black cod or halibut. Make sure to serve this with lots of white rice, which is your soluble fiber foundation for this meal. The rice is also perfect for sopping up the delicious glaze!
Makes 2 servings, easily doubled
2 tablespoons maple syrup
2 tablespoons soy sauce or tamari
1 1/2 tablespoons fresh lemon juice
2 teaspoons whole grain Dijon mustard
1 tablespoon Acacia Tummy Fiber (for extra soluble fiber, and a great emulsifier!)
1 tablespoon water
2 tablespoons toasted sesame seeds
2 six-ounce tuna steaks (or salmon, halibut, black cod)
2 teaspoons sesame or olive oil
Jasmine or basmati rice for serving
In a small bowl whisk together first 6 ingredients and set aside. Spread sesame seeds evenly in a pie plate. Coat the tuna steaks with the crushed seeds. In a large non-stick skillet heat oil over medium heat, and cook tuna steaks 3-4 minutes per side, until golden and just cooked barely through. Transfer tuna to serving plates. Add glaze to hot skillet and simmer one minute, then pour over tuna. Serve with rice.
The perfect drink with this dinner is a hot cup of Fennel Tummy Tea!
Are you just learning how to eat for IBS? A little intimidated at the thought of special IBS recipes? Not quite sure just what makes these recipes special in the first place? Don't worry! Get Eating for IBS and find the answers to all your questions.
~ Heather's Tummy Fiber ~
For the Dietary Management of IBS Pain, Diarrhea, &, Constipation

Certified Organic Acacia Senegal ~ Pure Soluble Fiber
The prebiotic fiber that relieves both diarrhea and constipation!
** Very Economical **
** 100% Acacia Senegal ** Never Low Grade Acacia Seyal
 Don't Go Anywhere Without Them!
Don't Go Anywhere Without Them!
This is just to THANK Heather for all her insights and helpful support. Her latest email What If You Fall Off The IBS Wagon? was very encouraging, as are all her pearls of wisdom.
And, Heather's Tummy Teas are my don't-go-anywhere-without-them beverages of choice since I discovered this website two years ago. Thanks for everything!
I've told many people about not only the teas but also the basic eating guidelines, all of which have helped me beyond words. So, yep!
Gratefully,
Andrea G.
Oh my gosh, Andrea, I'm truly blushing! I am so happy you are feeling better! ~ Heather
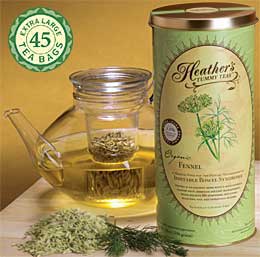  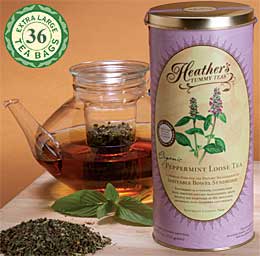
Organic High Volatile Oil Fennel & Peppermint Tummy Tea Bags
Extraordinary Quality ~ Very Economical
Fennel is terrific for bloating & gas, Peppermint is great for IBS pain & spasms.
Heather's Fennel Tummy Tea Heather's Peppermint Tummy Tea
  
Compare for yourself! The pictures above show the huge difference in the quantity and quality of tea per teabag.
 Soy Foods Protect Against Colon Cancer
Soy Foods Protect Against Colon Cancer
University of Illinois scientists have evidence that lifelong exposure to genistein, a bioactive component in soy foods, protects against colon cancer by repressing a signal that leads to accelerated growth of cells, polyps, and eventually malignant tumors.
The cells in the lining of the human gut turn over and are completely replaced weekly. However, in 90 percent of colon cancer patients, an important growth–promoting signal is always on, leading to uncontrolled growth and malignancies.
This study suggests that the aberrant signaling during the development of colon cancer can be regulated by soy–rich diets. A diet rich in soy genistein represses those signals through epigenetic modifications at the regulatory regions of those genes.
Go here for full research article.
Is Going Gluten-Free Right for You?
The Academy of Nutrition and Dietetics has said that three types of people may not be able to eat gluten: people with celiac disease, people with gluten sensitivity or intolerance, and people with a wheat allergy.
Celiac disease is an autoimmune disorder, and when gluten is eaten, the body triggers an attack on the intestines. Damage occurs over time, and nutrients can't be absorbed. For someone with celiac disease, it's critical that there is zero exposure to gluten.
Another group of people who might benefit from forgoing gluten are those who have what's called gluten sensitivity. This non-celiac-related sensitivity to gluten is just starting to be recognized and researched. Gluten triggers symptoms, but there is no visible damage to the intestine. It's not yet known if there are any long-term consequences of gluten sensitivity.
Others who might want to avoid gluten are those who are allergic to wheat. There's no specific allergy to gluten, but some people with a wheat allergy choose to avoid gluten-containing products altogether due to the risk of cross-contamination with wheat.
Though it might seem logical to stop eating gluten to see if it's at the root of your problems, that's an extremely bad idea. First see a gastroenterologist to be evaluated for celiac disease. Otherwise, stopping consumption of gluten can mask the true cause of your symptoms.
Once those results are in, dietary adjustments can follow. The best gluten-free diet is one that contains foods that are naturally gluten-free, such as fruits, vegetables, low-fat dairy, beans, nuts, seeds, fish and lean meats.
Go here for full research article.
How Does Peppermint Help Relieve Irritable Bowel Syndrome?
University of Adelaide researchers have shown for the first time how peppermint helps to relieve IBS, which affects up to 20% of the population. Researchers from the University's Nerve-Gut Research Laboratory explain how peppermint activates an "anti-pain" channel in the colon, soothing pain in the gastrointestinal tract.
Their research shows that peppermint acts through a specific anti-pain channel called TRPM8 to reduce pain sensing fibers, particularly those activated by mustard and chilies. This is potentially the first step in determining a new type of mainstream clinical treatment for IBS.
IBS is a gastrointestinal disorder, causing abdominal pain, bloating, diarrhea and/or constipation. It affects many people on a daily basis, twice as many women as men.
Go here for full research article.
~ Heather's Tummy Tamers Peppermint Oil Capsules ~

Peppermint Oil Caps Called "Drug of Choice for IBS"
Our Peppermint Oil Caps have the added benefits of fennel and ginger oils, and they help prevent abdominal pain, gas, and bloating!
 Hormones and IBS - Menstruation, Pregnancy, Menopause, and More. Hormones and IBS - Menstruation, Pregnancy, Menopause, and More.
Most women with IBS suspect that hormone fluctuations affect their IBS symptoms, and research has shown this to be true - quite dramatically true. Women have a higher prevalence of IBS than men in the first place. This may be due to sex-related differences in brain responses to visceral (body) and psychological (mind) stressors, as well as hormonal influences.
Women with IBS have more severe symptoms and need more medications than men. Small-bowel transit, gastric emptying, and colonic transit times are all significantly different for women (even women without IBS) than for men. and hormones are believed to play a large role here.
There are even estrogen receptors in the stomach and small intestine, which react to changing levels of hormones.
Periods? Bad News...
Most women with IBS quickly learn through experience that menstruation leads to worse IBS pain and bloating, and increased bouts of diarrhea as well. The high progesterone levels that trigger menstrual cramps can also cause bowel spasms. This makes sense, as both the uterus and the bowel are smooth muscle tissue - but it's a really unfair experience for many women, who have to endure painful IBS cramps on top of painful menstrual cramps.
Not surprisingly, studies show that three-quarters of women with IBS say their symptoms are worse during their periods.
For many women, taking steps to prevent or relieve menstrual cramps can help prevent period-related IBS symptoms as well. Regular exercise (especially yoga), direct heat on the lower abdomen, and herbal teas with smooth muscle relaxant properties can all be very helpful.
A brand new study just proclaimed that fennel is an effective herbal drug for menstrual pain. This is terrific, because fennel is already known for its carminative (gas and bloating relief) benefits for IBS. This makes fennel a double whammy for cramps and IBS in the best way.
For some women, birth control pills and hormone-releasing IUDs can lessen menstrual symptoms and associated IBS flares - this is an issue to address with both your GI doc and your ob/gyn.
Pregnancy? Could Go Either Way...
Research shows that pregnancy can have a significant impact on IBS, but there is no consensus as to what that impact will be. The extreme hormonal fluctuations of pregnancy often trigger GI distress in women who do not even have IBS. For those who have a dysfunctional gut to begin with, predicting whether IBS will worsen or improve during pregnancy is a bit of a coin toss.
It's not uncommon for pregnant women to feel that their IBS has completely gone into remission, but the flip side of that coin is that other women may feel that pregnancy makes their IBS worse than it has ever been before. Or, the severity of IBS symptoms may stay the same while the symptoms themselves change - someone who is normally diarrhea-predominant will suddenly be constipated, or vice versa. Gas and bloating may worsen one month while abdominal cramps disappear, but the next month the opposite happens.
This inconsistency can happen not just within the term of a single pregnancy, but women can also have dramatically different experiences with their IBS from one pregnancy to another.
For a note of reassurance here, remember that pregnancy seems just as likely to affect IBS for the better and not automatically for the worse. Also keep in mind that, to my knowledge, there is no evidence at all that IBS has any effect whatsoever on a woman's ability to conceive and carry a full-term, healthy pregnancy with normal delivery. I don't know of any reason why IBS should compromise your wish to have children - and your own ob/gyn should be able to address all of your concerns here.
Menopause? Good News!
The research on IBS and menopause is fortunately clearer and more optimistic (yay!). Studies have shown that the drop in hormones after menopause results in reduced severity of IBS symptoms. After age 50, the severity of IBS symptoms in women and men is identical.
Women in postmenopausal age groups have significantly less IBS abdominal pain and bloating, and have higher quality of life scores compared to younger women with IBS. The theory that the drop in hormones from menopause directly correlates with improved IBS symptoms is further supported by studies finding that hormone replacement therapy in menopause is associated with an increased risk of IBS flares.
So, while hormones and gender do play a significant role in IBS (possibly the development of the disorder as well as the severity and frequency of symptoms), it's not all bad news.
IBS flares from menstruation can be well-managed with healthy lifestyle adjustments, many of which overlap with benefits for both IBS and menstrual cramps. Pregnancy seems to be at least as likely to improve symptoms instead of worsen them, and if pregnancy does trigger more IBS attacks there is nothing to show that this won't completely subside after childbirth. Menopause is clearly linked to significant improvements in IBS across the board.
Hormonal fluctuations that affect IBS for the worse are typically temporary, with no serious or permanent health consequences. As is the case with so many other elements that affect IBS, arming yourself with as much knowledge as possible is one of the very best ways to manage your symptoms from the outset. You can successfully control your IBS - IBS does not have to control you.
To read through a wealth of research findings on hormones, pregnancy, and menopause in IBS, including all of the studies referred to above, go to the gender section of the IBS Research Library.
~ Heather

Shop at Heather's Tummy Store for IBS
HelpForIBS.com
The only store that's just for IBS - so we only carry the very best

You're on this newsletter list because you have expressed interest in IBS news and information.
Unsubscribe Here
Change your newsletter email address here.
If you are viewing this newsletter on a website and would like to subscribe for email delivery, please "Join the IBS Newsletter" here.
ANTI-SPAM PRIVACY & SECURITY POLICY
HelpForIBS.com
Heather's Tummy Care
80 S. Washington St, #304
Seattle, WA 98104 USA
© 2013 Heather Van Vorous, Heather's Tummy Care. All rights reserved.
Authored by Heather Van Vorous. May not be reproduced without permission.
USA Copyright Office Registration Number TXU 1-270-858 and others.
|
|
| |