| |
 |
Certified Organic
Acacia Tummy Fiber
The prebiotic 100% soluble fiber that relieves both diarrhea and constipation!
In this Issue...
Food & Recipes
Special Letters
Rx News & Research
Ask Heather
Did you miss the latest
IBS newsletter, and how
Bloating & Constipation Disappear?
Past issues
are posted here!
|
 |
|
| |
Heather's IBS Newsletter ~ For Irritable Bowel Syndrome
June 26, 2007
Skeptical but Amazed ~ How Linda is 90% Better After Just 2 Weeks!
Hello to everyone ~
Welcome to a very special memorial issue of the IBS newsletter, and an exceptionally personal one for me. As anyone who has read the books Eating for IBS or the First Year: IBS knows, I was raised by my wonderful grandparents, and many of my IBS-friendly recipes came out of meals I grew up cooking with my Grams.
As I developed IBS at age 9 and received no help from my pediatrician whatsoever, it was the support and caring of my grandparents that enabled me to learn how to successfully overcome my symptoms and lead a normal, healthy, happy life.
They made this possible for me when I was still a child, and newly struggling with these horrible, mysterious symptoms that doctors were telling me were all in my head. They also never stopped encouraging me as an adult, and remained my proudest supporters as I moved from being a patient to an advocate for others with IBS.
Last week my grandfather died, so I would like to dedicate this issue to him. If I can offer all of you the help, caring, and support with your IBS that he offered me, the world will be a better place for us all.

Bumpa, Grams, and me
Best Wishes,
Heather Van Vorous
Did a friend send you this newsletter? Sign up here for your own free subscription. 
Lemon-Glazed Sticky Bread My grandfather loved anything lemon, and this bread was one of his favorites. It's tart, sweet, and intensely lemony. Though it's luscious and rich, it's also dairy-free and low fat. This bread is the perfect example of a recipe that is so delicious it will be loved by people who don't even have IBS - even though it's perfectly safe for those of us who do.
Don't forget the glaze - the bread just isn't the same without it.
Makes One 9 x 5" loaf, 16 slices per loaf
3/4 cup soy/rice milk
2 teaspoons apple cider vinegar
2 cups all-purpose unbleached white flour
2 tablespoons Acacia Tummy Fiber
1 1/2 teaspoons baking powder
1/2 teaspoon salt
1 1/2 cups granulated sugar
1/4 cup plus 2 tablespoons canola oil
4 organic egg whites
zest from 2 lemons, minced
Glaze:
strained juice from 2 lemons
3 tablespoons granulated sugar
Preheat oven to 350 F. In a medium bowl add vinegar to soy milk and stir well (this will clabber, or "sour" the milk); set aside.
Sift dry ingredients into large bowl. Whisk well to combine.
Add to clabbered soy milk the oil, egg whites, and zest. Whisk well until thoroughly combined.
Add wet ingredients to dry with a few swift strokes by hand just until blended. Pour batter into a non-stick loaf pan sprayed with cooking oil. Bake for about 1 hour or until a toothpick or cake tester inserted into the center of the loaf comes out clean.
While bread is baking, stir glaze ingredients together until sugar dissolves. When bread is done, and while it is still hot from the oven, run a sharp knife around the edges of the pan to loosen the loaves, and prick bread carefully all over with a thin wooden or metal skewer. Pour glaze over bread, and cool in pan on rack. Bread is even better the next day.
For a lovely summer afternoon snack, have a slice of lemon bread with a cup of lightly sweetened Peppermint Tummy Tea.
Are you just learning how to eat for IBS? A little intimidated at the thought of special IBS recipes? Not quite sure just what makes these recipes special in the first place? Don't worry! Come see the IBS Diet pages, and find the answers to all your questions.
Organic High Volatile Oil Fennel & Peppermint Tummy Tea Bags
Extraordinary Quality ~ Very Economical
Fennel is terrific for bloating & gas, Peppermint is great for IBS pain & spasms.
 Much to Her Surprise, She is 90% Better
Much to Her Surprise, She is 90% Better
Dear Heather,
Thank you, the Fennel Tummy Tea arrived on Saturday. I appreciate such quick service.
To be honest, I really didn't expect such excellent results from your products. I had hoped for some improvement. After having IBS for twenty years, I didn't expect a miracle. I guess I am a skeptic.
Much to my surprise, they worked as well as they were advertised. I couldn't use them the way you recommended, gradually switching from medicines to natural solutions. Instead, I was taking Zelnorm, and had to stop taking it immediately.
Much to my amazement after two and half weeks of taking Acacia Tummy Fiber and drinking the Tummy Teas my problem is about 90% improved. I imagine after a month I should have no problems at all.
You are welcome to use my comments. You can note that I'm in Japan if you wish – just so people know there is no place in the world where people really know or care about IBS.
Linda Reinherz
Ami Machi, Japan
Thank you so much, Linda. I'm so glad you took a chance and are now feeling better! ~ Heather
Did you miss the recent letter from Cheryl, whose bloating and constipation disappeared and life completely turned around?
~ Heather's Tummy Fiber ~
For the Dietary Management of Abdominal Pain, Diarrhea, &, Constipation

Certified Organic Acacia ~ Pure Soluble Fiber
The prebiotic fiber that relieves both diarrhea and constipation!
** Very Economical ** Only 3 cents per gram of fiber!
 Overlapping Upper & Lower GI Smptoms in IBS
Overlapping Upper & Lower GI Smptoms in IBS
A study in the American Journal of Gastroenterolgoy noted that distinguishing between irritable bowel syndrome (IBS) and functional dyspepsia can be challenging because of the variations in symptom patterns, which commonly overlap. However, the overlap is poorly quantified, and it is equally uncertain whether symptom patterns differ in subgroups of IBS arbitrarily defined by primary bowel patterns of constipation (IBS-C) and diarrhea (IBS-D). The study found that IBS-C patients reported significantly more overall GI symptoms when compared to patients with IBS-D. Abdominal pain patterns differed in patients with IBS-C versus IBS-D. Bloating was substantially more common in IBS-C patients. The study concluded that upper GI symptoms consistent with functional dyspepsia were more frequent in IBS-C. Although there was considerable overlap of upper and lower GI symptoms in patients with IBS-C and IBS-D, the former had more frequent lower abdominal pain and bloating.
Go here for more information about this study...
Antidepressant Therapy NOT Effective for Irritable Bowel Syndrome?
A recent study in Digestive Diseases and Sciences noted that the efficacy of antidepressants in irritable bowel syndrome (IBS) is controversial, and that no trials had directly compared a tricyclic with a selective serotonin reuptake inhibitor. This study's aim was to determine whether imipramine (Tofranil) and citalopram (Celexa) are efficacious in IBS. This was a randomized, double-blind, placebo-controlled, parallel group pilot trial. The majority of patients were diarrhea-predominant. The study concluded that neither imipramine nor citalopram significantly improved global IBS endpoints over placebo. Go here for more information about antidepressants and IBS...
Go here for more information about this study...
Have your personal experiences mirrored the findings of this study, or have your IBS symptoms been helped by antidepressants? Share your experiences on the IBS Message Boards.
Is There Any Food I Can Eat? Living with IBD and/or IBS
A small but provocative study in Clinical Nurse Specialist addressed inflammatory bowel disease (Crohn's disease and ulcerative colitis) and irritable bowel syndrome, noting that both of these GI conditions significantly impair quality of life and the ability to complete activities of daily living. Unfortunately, there has been little education and research surrounding the evaluation of effective coping strategies with respect to GI disorders, particularly from the perspective of those diagnosed.
The overall objective of this research was to explore the lived experience of women who had been diagnosed with inflammatory bowel disease and/or irritable bowel syndrome. This article specifically explores the relationship between food and irritable bowel syndrome and/or inflammatory bowel disease. Qualitative information was collected in the form of background questionnaires, e-mail interviews, and face-to-face interviews, which were subsequently analyzed for trends.
Every woman reported that one of the most significant means by which to cope with their condition centered around food consumption or controlling their food consumption. Subjects identified the importance of determining their "trigger foods," selecting healthy food choices, the impact of stress, and problems associated with food and travel.
This research, predicated on the narratives of women diagnosed with GI disorders, substantiates the profound effect that food has on conditions of the GI tract. All of the women identified their relationship with food as a dynamic learning process, one that they thought would be a lifelong struggle. Go here for comprehensive information about managing IBS through food and diet...
Go here for more information about this study...
Looking for more IBS research and news? Check the IBS Research Library!
~ Heather's Tummy Tamers Peppermint Oil Caps ~For the Dietary Management of Abdominal Pain &, Bloating

Peppermint Oil Caps with Fennel and Ginger Are Amazing!
Our Peppermint Oil Caps have the added benefits of fennel and ginger oils, and they help prevent abdominal pain, gas, and bloating!
 Children, Doctors, and IBS ~ A Very Personal "Ask Heather" Children, Doctors, and IBS ~ A Very Personal "Ask Heather"
"My child probably has IBS and has several doctors' appointments coming up. How can I help? "
As difficult as it can be to manage IBS as an adult, I can say from personal experience that it is without a doubt more difficult to deal with as a child. One of the scariest and most stressful aspects for a child is seeing doctors. Having a parent who can make the ordeal less traumatic, and more productive, is critically important. I certainly would never have made through my childhood at all without the support of my grandparents, who did everything possible to minimize the terror of numerous doctor (and even emergency room) visits.
However, as a parent, you have to walk a fine line when your child visits a doctor for GI tract problems. By necessity you must be intimately involved with your child's health care and deal with their doctors first-hand, but the normal way you'd go about this may be in direct conflict with how your child wishes to handle the situation.
Children are likely to have a very strong preference in one of two ways. They may insist that you stay right next to them throughout the examination and every single diagnostic test that follows, and in this case it's easy to comply. However, your child may instead be much more comfortable talking alone with the doctor and having you out of the room. As well as you think you know your child it's best to not make an assumption here (don't even judge from past doctor's visits – IBS can be a whole different ballgame).
It's a good idea to casually ask your child if they'd rather you stayed in the waiting room when they see their doctor, and make it clear that you'll understand how they feel (and won't be hurt) if they say yes. It may be difficult to even get a straight answer from your children in this matter. They may be so embarrassed and just plain exhausted by IBS that they'll give whatever answer they think will make you drop the subject as quickly as possible. So approach them at a quiet, low-key time when there's no one else around to overhear, give them a hug, ask them what they'd like your role to be when they see the doctor, and make it clear that you will let them call the shots here. Anything that can be done to minimize the trauma of the experience will help children tremendously. To them, talking to a doctor at all is much scarier than it is for an adult. To talk about bowel movements with a doctor is truly a nightmare. Whatever steps you can take to make things emotionally easier will earn you your child's undying gratitude.
I really can't stress enough how embarrassing IBS can be to a child, and having to describe symptoms in detail to a total stranger while sitting half-naked in a paper gown is very traumatic. For me, having my parents with me in that situation just compounded my humiliation. They were very kind, concerned, and supportive, but their presence took away any last shred of privacy I had left in dealing with the problem. Even as a teenager I was much more comfortable meeting with my doctor and enduring the diagnostic tests alone, though I very much wanted my parents right outside in the waiting room the entire time. Fortunately, they were understanding in this matter, and helped minimize the stress of the situation for me tremendously. They simply met with the doctor alone when I was through. In this way they stayed well-informed and I felt a little less stripped of all dignity by the whole ordeal.
From the vantage point of an adult, my feelings as a child seem inexplicable and frankly rather strange. Nowadays, I wouldn't care less if my parents were with me at the doctor's, and their presence certainly wouldn't seem to be an invasion of privacy but a supportive presence. However, this was definitely not how I felt as a child, and my feelings then, no matter how odd they seem today, were very real. I remember the heat of them quite vividly, and I remain thankful that my parents treated them as legitimate.
Any good doctor will respect children's feelings as well, and make the extra effort necessary to put them at ease. You may want to visit a pediatric gastroenterologist, as a doctor who deals exclusively with children should be more likely to understand their quirks and accommodate them. To this day I am grateful to the doctor who finally diagnosed me at age 16, as he requested on his own that my parents wait outside the examining room, and this immediately set me at ease. (In hindsight his actions make me suspect he'd had his share of young patients and knew from experience just how to successfully deal with them).
He then told me straight-out that every patient he sees feels embarrassed to be there, and that most people are very reluctant to discuss the type of health problems he deals with every single day. He made it clear that the whole topic was very routine to him, that I had nothing to be embarrassed about, that everything I told him he would take seriously, and he then stressed that he really needed to get detailed information from me or he couldn't help. He asked me very specific, yes-or-no questions to "warm me up" to the topic before expecting me to give full-blown descriptions of my attacks. This was the perfect approach for him to take with me, and your child's doctor should strive to find an approach that works equally well. If the doctor can't or won't help your child in the way they need to be helped, move on to a new doctor.
~ Heather
Did you miss the recent "Ask Heather" about summer weather and IBS? Find it here...
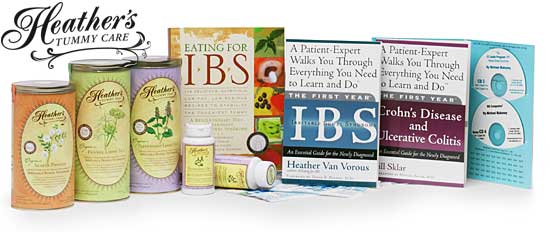
Shop at Heather's Tummy Store for IBS
HelpForIBS.com
The only store that's just for IBS - so we only carry the very best

You're on this newsletter list because you have expressed interest in IBS news and information.
Change your newsletter email address here.
If you are viewing this newsletter on a website and would like to subscribe for email delivery, please "Join the IBS Newsletter" here.
ANTI-SPAM PRIVACY & SECURITY POLICY
HelpForIBS.com
Heather's Tummy Care
80 S. Washington St, #304
Seattle, WA 98104 USA
© 2007 Heather Van Vorous, Heather's Tummy Care. All rights reserved.
USA Copyright Office Registration Number TXU 1-270-858 and others
|
|
| |